Managing a Difficult Infection
by Marybeth Spanarkel, M.D., on November 15, 2019
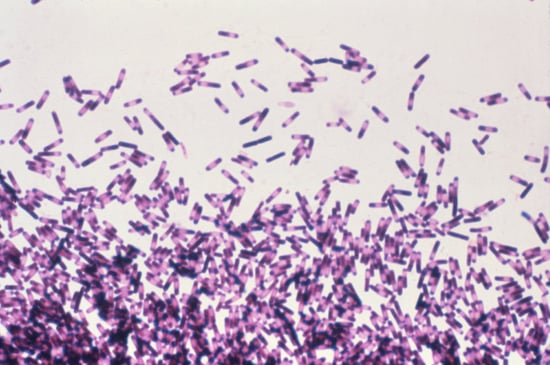
The “difficile” in Clostridium difficile is a French word meaning “difficult.” The name choice was no accident. C. diff, now known as Clostridiodes difficile, is the most common hospital-acquired infection, with 453,000 cases and 29,300 deaths reported annually. Since 2000, there has been a marked increase in the number and severity of cases.
A Tenacious Infection
The C. diff infection (CDI) causes symptoms ranging from mild diarrhea to severe colon inflammation, and as noted, can be fatal. The disease stems from clostridoides bacteria that, when ingested, will produce toxic spores under certain conditions. Infected individuals then excrete these hardy, difficult-to-eradicate spores, which can be transmitted to others.
Because of their tendency to destroy even healthy, protective bacteria in the gut, the major risk factor for CDI is the use of antibiotics. However, even healthy individuals who have not taken antibiotics can develop CDI. Other risk factors include advanced age, a weakened immune system, other GI illnesses (e.g., Crohn’s disease or ulcerative colitis), chemotherapy, being in a hospital or a long-term care facility, and the use of acid-suppressive medications.
CDI Treatment Options
In terms of treatment, the first step is, if possible, to stop the antibiotic that triggered CDI. The second step is administration of an antibiotic that will kill C. diff. (e.g., fidaxomicin or vancomycin). Previously, flagyl (also known as metronidazole) was the first-line of treatment, but now over 30% of C. diff infections are demonstrating resistance to this drug. Most patients improve with 10 to 14 days of beginning treatment, but some are slow to recover, and about 20 to 40% will relapse.
For those patients with recurrent, relapsing CDI, fecal microbiota transplantation (FMT) is gaining popularity, with successful eradication in 80 to 90% of cases. In this procedure, after rigorous screening, donor stool is placed in the colon of the patient to restore a healthy bacterial environment. The FDA is working with various academic centers to coordinate safe trials of FMT.
C. Diff Is Preventable
In an endoscopy unit, contact with C. diff is likely at some point. Endoscopy staff (and any healthcare workers who are exposed to CDI) should scrub their hands with soap and water for at least 20 to 30 seconds before and after patient contact; note that alcohol gels do not inactivate spores. After an endoscopic procedure, surfaces should be thoroughly cleaned of visible contaminants and disinfected with an EPA-registered hospital disinfectant. It goes without saying that ASGE endoscope reprocessing guidelines should be rigorously followed. Finally, because spores can survive on dry surfaces for weeks and even months, endoscopy units should have a plan for cleaning and disinfecting the procedural space at the end of the day.

In general, promptly diagnosing patients allows for the implementation of control measures before the disease spreads. These measures include vigorous soap/hot water hand washing, quarantining patient to a private bathroom (when possible), using bleach-containing disinfectants for cleansing bathrooms, and hot water/bleach laundry washes. Finally, avoiding unnecessary use of broad-spectrum antibiotics is key for preventing further spread of CDI.
In view of the ever-increasing number of cases of CDI, adherence to patient-specific control measures is vital. Likewise, hospitals, particularly GI endoscopy units and intensive care units, should be uncompromising in their efforts to limit this potentially dangerous and persistent disease. These actions, in conjunction with evolving treatment modalities, are the key to reducing and eliminating this ”difficult” problem.


